Helicobacter pylori – curse or blessing?
Helicobacter pylori is a normal component of the gastric mucosa
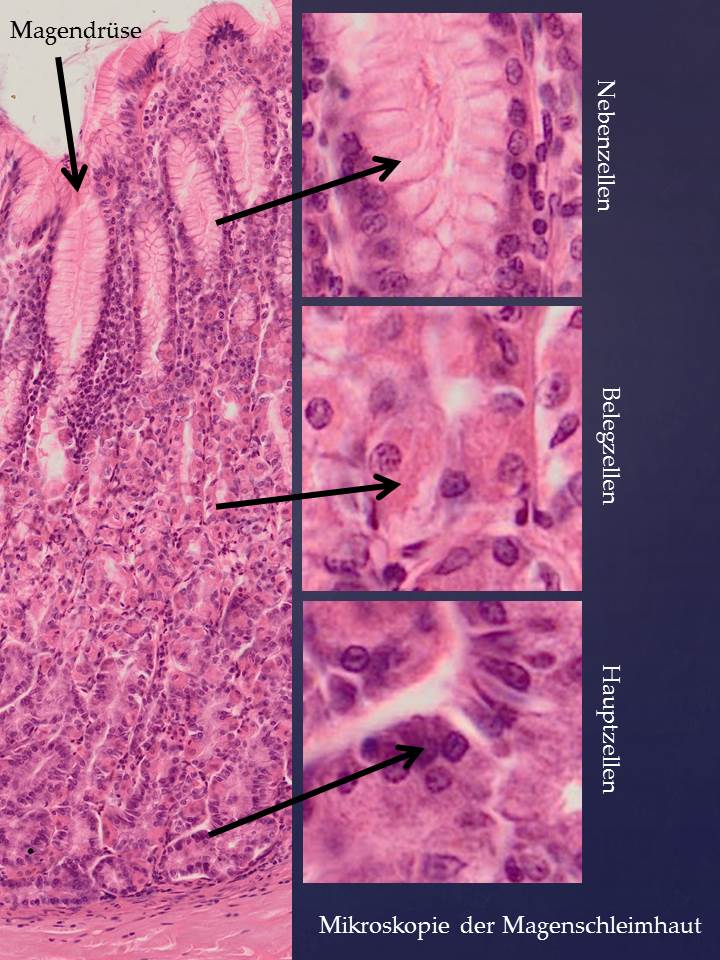
Helicobacter pylori (HP) is still regarded as a pathogenic germ that is even associated with the development of stomach cancer. In cases of inflammation of the stomach lining (chronic gastritis), a test is carried out which is almost always positive because HP is in fact a normal part of the microbiome in most Europeans. However, HP lives in the depths of the gastric glands. HP is acid-resistant and supports the formation of gastric secretions (metabolic products of HP contain neurotransmitters that stimulate gastric glands). HP is therefore actually a symbiont that is kept under control by the mucosal immune system.
The prevalence of Helicobacter pylori is often the result of malnutrition
In the case of dysbiosis, e.g. due to too many carbohydrates, especially sugar, HP slips out of this control and is then also on the surface of the gastric mucosa where it breaks down the layer of protective mucus that the secondary cells have formed. An excess of HP is therefore not necessarily the cause of a stomach disease, but often the result of malnutrition. An “eradication therapy” with antibiotics and acid blockers only provides short-term improvement, but does not eliminate the actual problem if the diet remains unchanged. Every antibiotic treatment affects the entire gut and changes the microbiome as a whole.
Proton pump inhibitors block parietal cells and lead to vitamin B deficiency
Modern broad-spectrum antibiotics inhibit protein formation in bacteria, but unfortunately also in mitochondria (which are similar to bacteria in many respects). Antibiotics destroy mitochondria in the cells of the intestinal mucosa, which are damaged as a result. The inhibition of gastric acid production by proton pump inhibitors (PPI), which are prescribed in addition to antibiotics, block parietal cells. This does improve symptoms such as heartburn and reflux. But the primary task of the acid is the hydrolysis of proteins. On the one hand, this is necessary for protein digestion; on the other hand, the enzymes of the stomach, especially pepsinogen, which is produced by the main cells, are not activated. This restricts protein digestion. In addition, parietal cells produce intrinsic factor, which is important for the absorption of vitamin B. Long-term use of PPI therefore leads to a vitamin B deficiency with all its consequences, such as altered blood formation.
An individual change of diet helps more sustainably
In the case of an acute infection, there is certainly no alternative to antibiotics and PPI. However, this treatment should be carried out very carefully and for a limited time. An individual change in diet is much more sustainable.
Further reading:
https://www.kallmeyer-naturheilpraxis.de/helicobacter-pylori-symbiont-erreger/
https://www.ncbi.nlm.nih.gov/pubmed/14567051
Author: Prof. Dr. Gustav Jirikowski, Faculty of Medicine, Jena
Find out more about the Cytolisa Immune Test and the nutrition program here